
Medical Credentialing Services
SERVICES BLSS MEDIX
Reduce Complicated Credentialing with our Medical Credentialing Services

Credentialing & Re-Credentialing
For healthcare providers, the process of Medical Credentialing is a nerve-racking task. With beyond 13 million medical practitioners currently operating in the U.S. along with the average practice length of about 40 years, insurance panels are swiftly becoming cramped and are slow to accept fresh medical providers into their network. BlssMedix is well-versed with all the industrial regulations and procedures, to navigate the provider credentialing process in order to accomplish rapid and positive outcomes. BlssMedix offers provider credentialing management service which encompasses filing documents for Hospital Privileging, Government Enrollments, Health Plan Paneling, CAQH and Licenses Expiry to aid new and existing individual providers and medical groups to ramp-up their profitability.
Credentialing is more than paperwork—it’s the foundation of your revenue. At Blss Medix, we help healthcare providers across the country navigate the complex, time-consuming credentialing process with speed, accuracy, and compliance. Whether you're launching a new practice, hiring new providers, or expanding your insurance panel, we streamline the process so you can start billing and getting paid without unnecessary delays.
Medicare
Health Partner
Medicaid

Credentialing is a Crucial Component
Many practitioners attempt to handle the process of medical provider accreditation internally. However, after examining the costs, the majority have discovered that outsourcing to BlssMedix is a sensible course of action.
Your efforts may be concentrated when you outsource your credentialing to a team of experts. Rather than having your staff credential one or two (or even twenty) providers at a time, BlssMedix’s team can handle it all at once, every day. This not only saves you money but also gives your team vital time to work on tasks that are more crucial to the development of your practice.
Credentialing is the verification process that allows healthcare providers to become approved by insurance companies, Medicare, and Medicaid to legally treat patients and receive reimbursements. It includes background checks, education verification, license validation, and insurance network enrollment.
Without proper credentialing, providers can’t get paid—regardless of how great their care is.
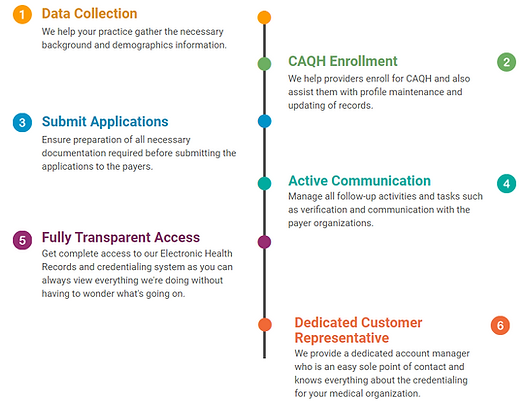
Our Credentialing Services Include:
-
Insurance Panel Enrollment
We enroll you with major commercial insurers, Medicare, Medicaid, and specialty plans. -
CAQH Profile Setup & Maintenance
Ensure your provider profile is complete, current, and ready for automatic payer pulls. -
Application Management
We complete, submit, and track every credentialing application for full visibility. -
Re-Credentialing & Maintenance
Stay in-network and avoid interruptions with proactive tracking and renewal services. -
Medicare & Medicaid Enrollment
We manage every step of your public payer applications from start to finish. -
Group & Solo Provider Credentialing
Whether you’re credentialing one provider or an entire group, we tailor the process. -
Contract Negotiation & Payer Communication
We liaise with insurance reps to ensure the best outcome for your network participation.


